How might we transform the experience of self-testing technology and connect it to other stakeholders in the system, so funding can be adopted and people at risk of late diagnosis choose to test more?
Project date: 2017 January - 2017 June
Project team: Developed in collaboration with John Makepeace
Project location: London
Project tutor: Nick de Leon, Ronald Jones
Those who supported us in the project: 56 Dean Street, Biosure, Dan Glass, Freedoms, Health Foundry, i-base, Kwa Africa, Mortimer Market Centre, Positive East, Terrence Higgins Trust.
My role: User researcher, Research analyst, Design strategist, Brand designer, UI/UX designer, Video editor.
>>
Project background
HIV HISTORY & EPIDEMIC
At its peak in the 90’s, many people died from AIDS because there was no effective treatment to control the disease. The idea that HIV and AIDS means death was deeply rooted in people’s minds in many forms from this period. Today, HIV is no longer a death sentence but a life sentence because the infection can be more controlled thanks to antiretroviral therapy (ART) which suppress the virus in your body sometimes even to the extent that it is non-transmissible.
AIDS epidemic in the 90s.¹ ²
LATE DIAGNOSIS OF HIV
The enduring issue of HIV is late diagnosis which is when someone has been diagnosed after the virus has already significantly damaged their immune system. In 2015, 39% of those diagnosed were late. (2035/6028 people)³ The impacts are extreme:
The costs of HIV care are 50% more for each year after diagnosis.⁴
People are 3 times more likely to pass on the infection.⁵
In 2013, 81% of all AIDS-related deaths were caused by late diagnosis.⁶
There are still 13,500 HIV+ people who are undiagnosed.⁷ They represent a threat in funding terms of £1.25bn extra if they don’t get diagnosed soon.⁸
>>
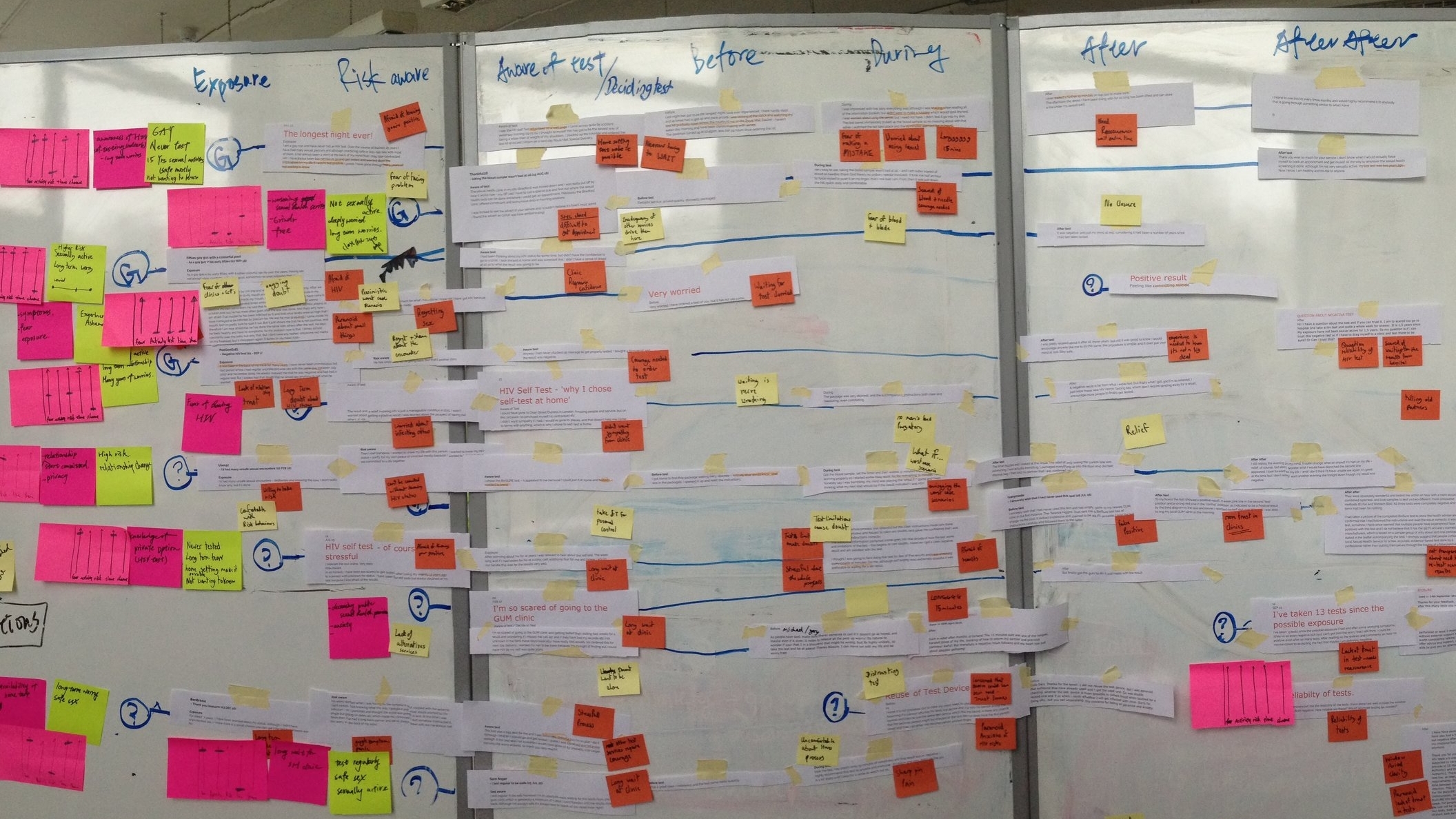
The research
To understand every aspects of HIV/AIDS issue, we have
interviewed 8 HIV positive people and 15 experts from sexual health clinics, HIV campaigns/ testing/ prevention/ care/ research organisations.
joined 4 HIV outreach testing sessions with Positive East.
studied 2 online HIV support forums and various reports relating to late diagnosis of HIV, HIV stigma & discrimination, HIV in different ethnicities/ communities, HIV prevention/ testing/ care support etc.
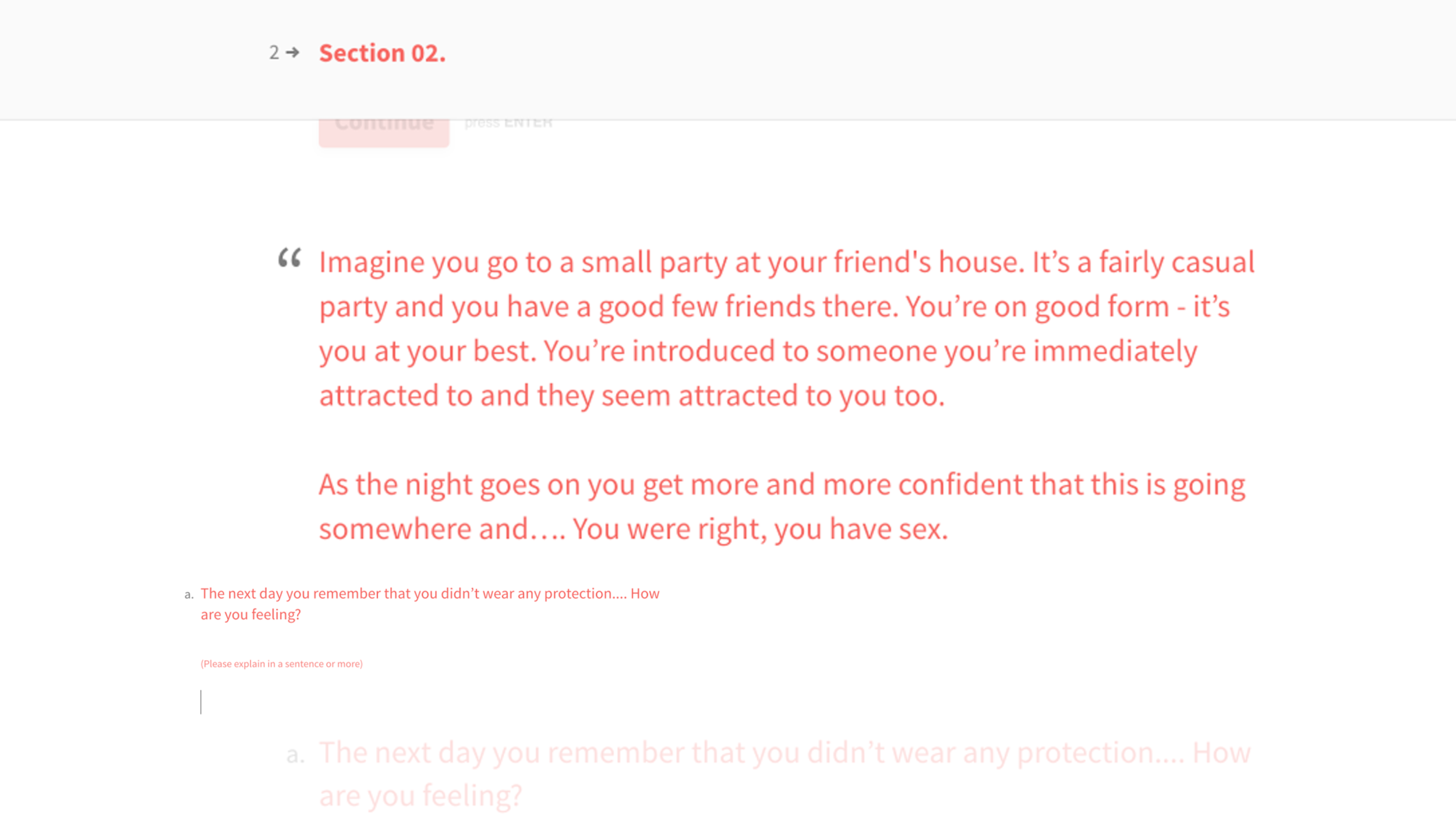
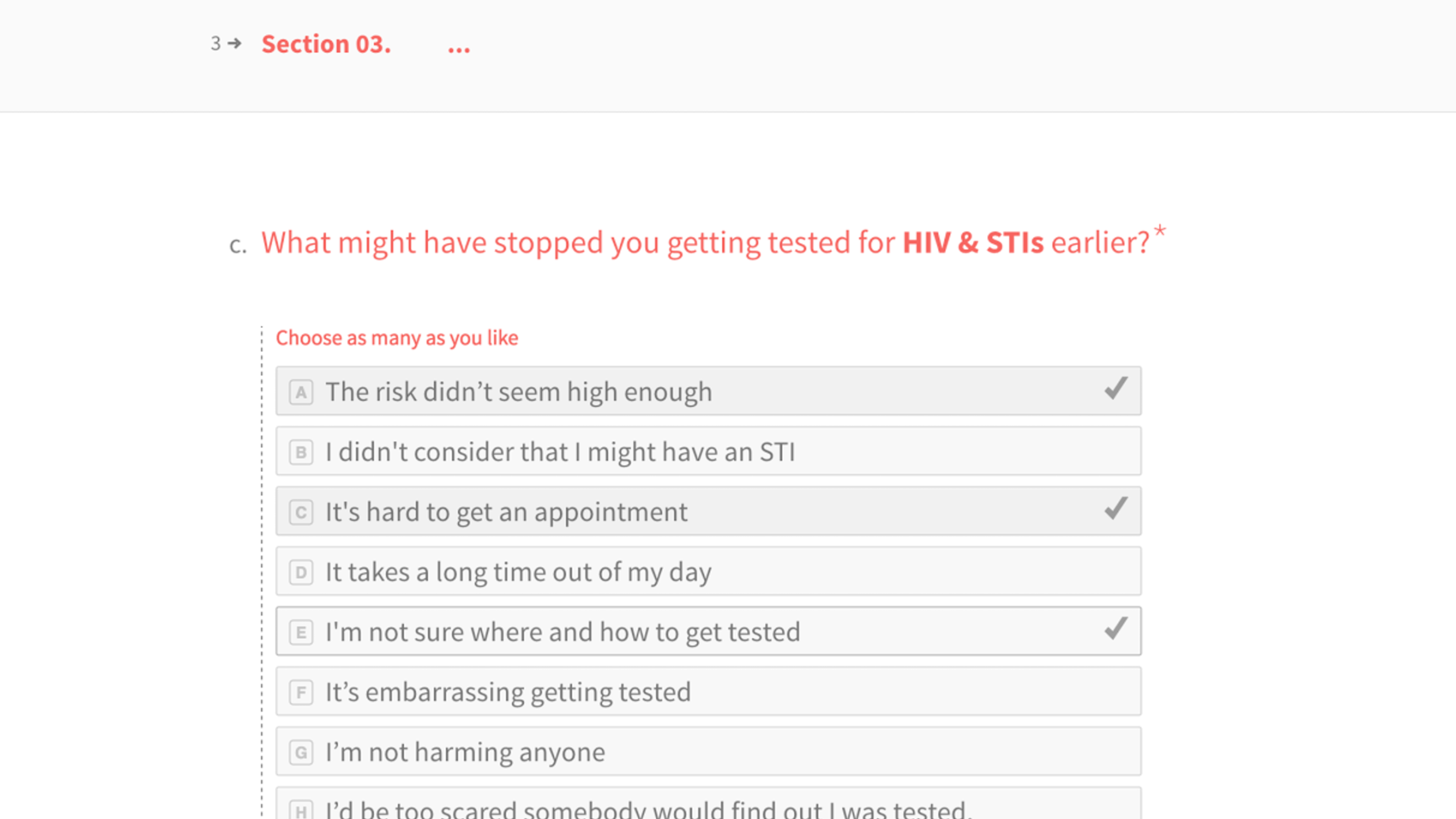
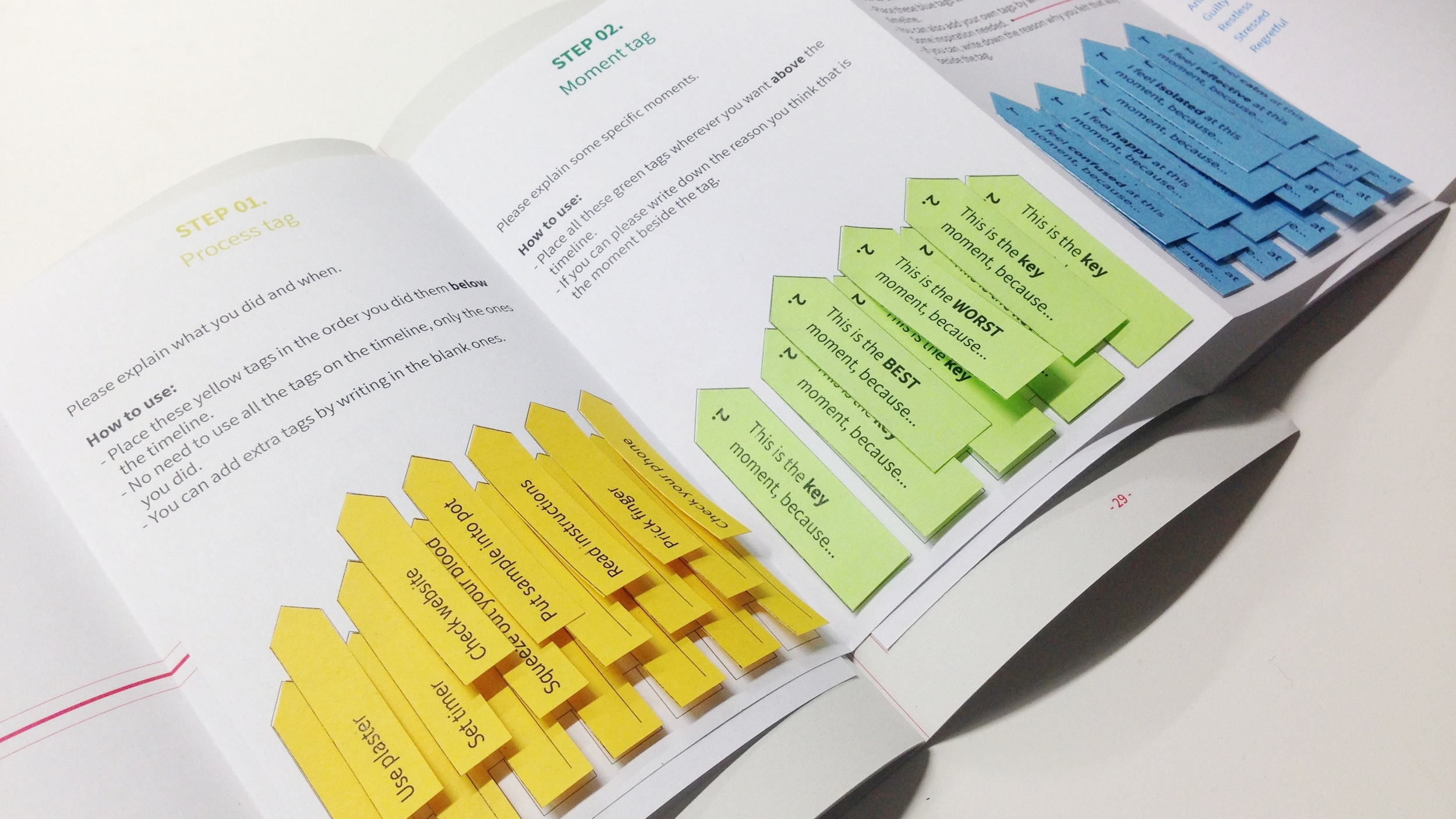
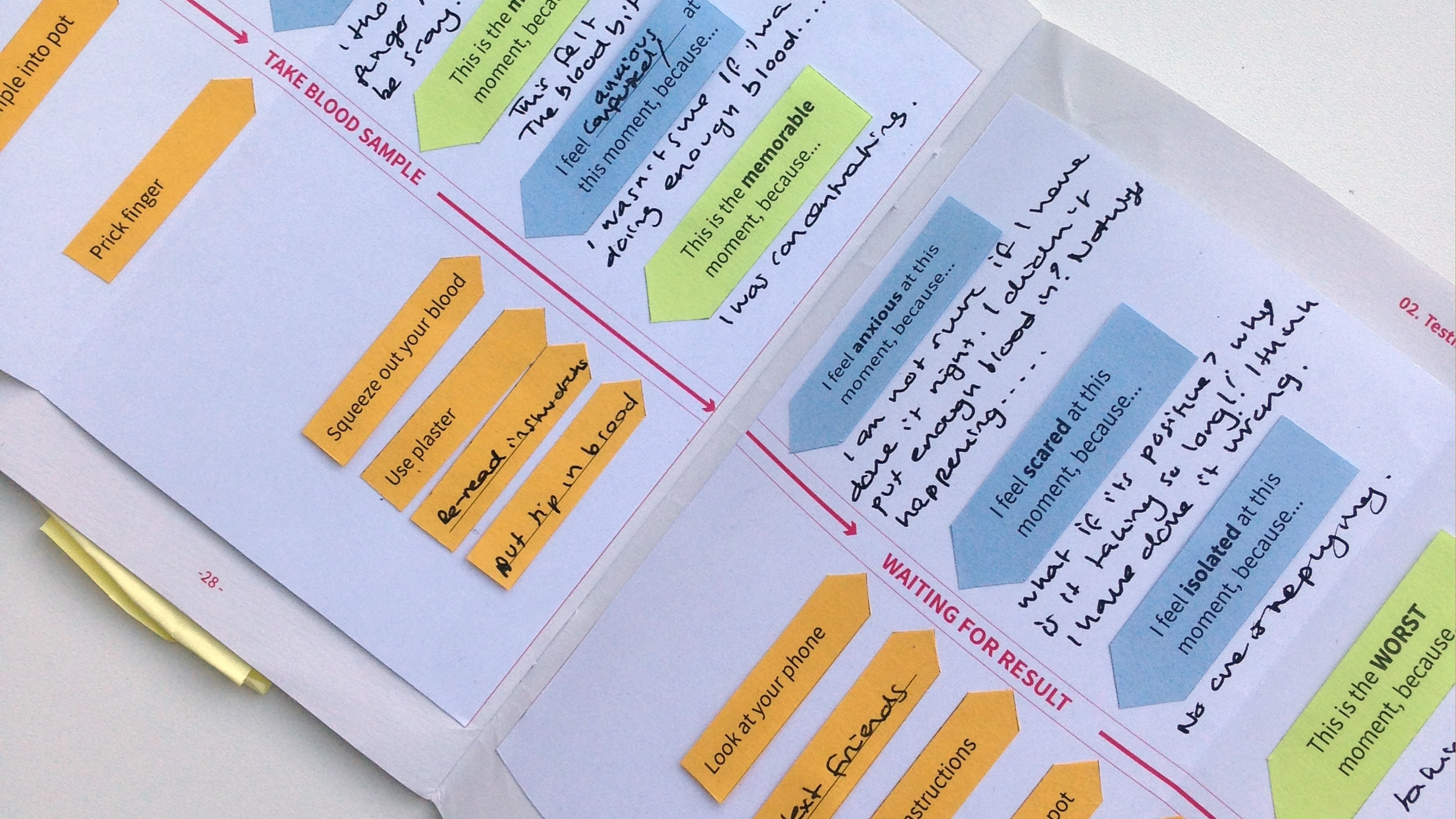
done 36 online surveys and 11 self-testing research probes.
>>
Key insights
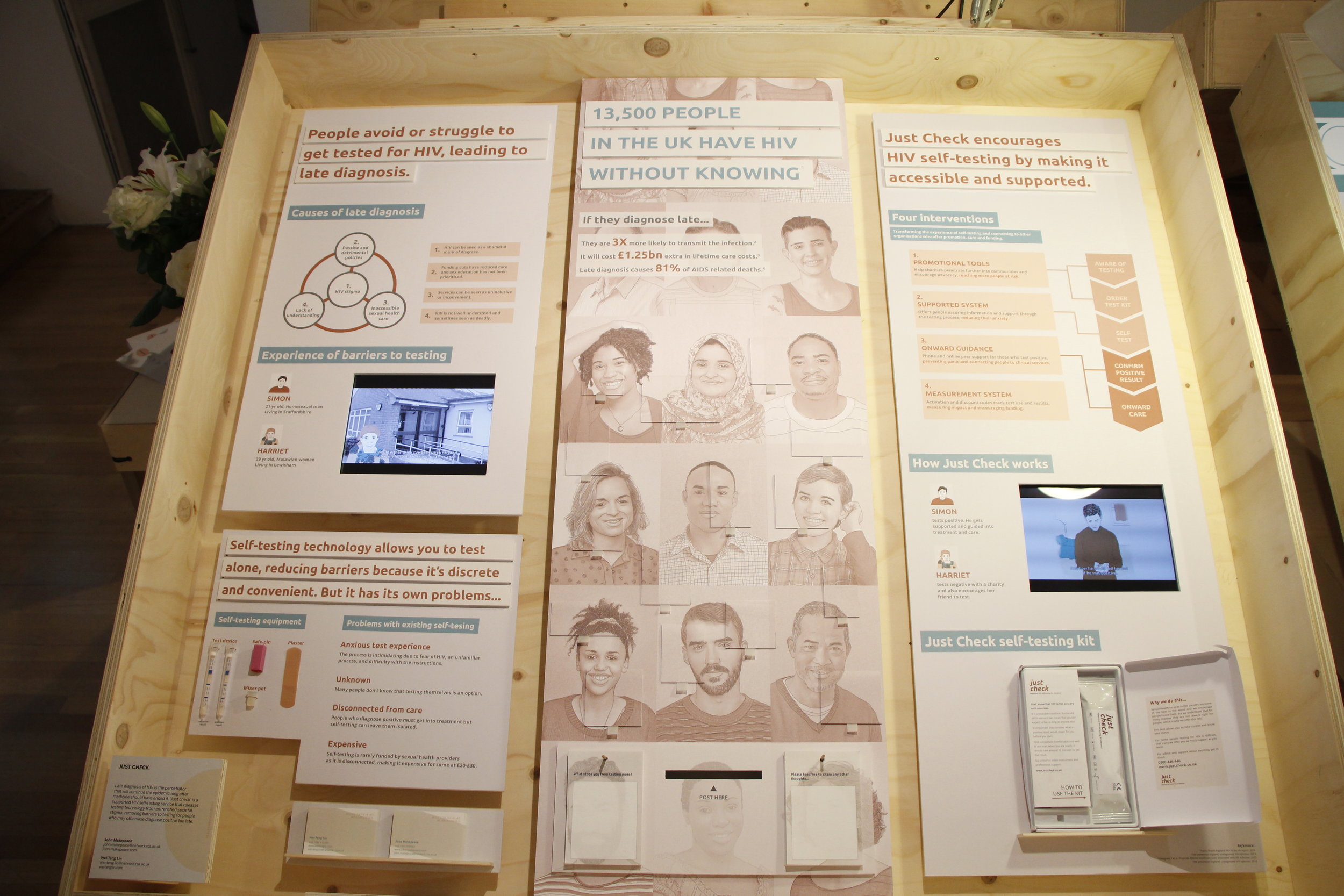
CAUSES OF LATE DIAGNOSIS
People avoid or struggle to get tested for HIV leading to late diagnosis because...
Stigmatised sexuality: Our sexual identities can create a sense of shame. Sexual health issues are seen as a mark of abnormal sexual behaviour, HIV more than most.
Passive & Detrimental policy: Policy has not prioritised sex education and has reduced sexual health resources.
Un-inclusive sexual health services: Sexual health care can be perceived as un-inclusive, inconvenient, untrustable, inexperienced or prejudiced.
Lack of understanding: Information is poorly handled stunting the growth of understanding about sexuality and sexual health.
The two stories below demonstrate how these issues unfold into barriers that people face.
Simon, 21 yrs old, homosexual man, living in Staffordshire.
Harriet, 39 yrs old, Malawian woman, living in Lewisham.
PROBLEMS OF SELF-TESTING
Self-testing technology allows people to test alone reducing barriers because it is discrete and convenient. But it has its own problem:
Anxious test experience: The process is intimidating due to fear of HIV, an unfamiliar process, and difficulty with the instructions.
Unknown testing option: Many people don’t know that testing themselves is an option.
Disconnected from care: People who diagnose positive must get into treatment but self-testing can leave them isolated.
Expensive: Self-testing is rarely funded by sexual health providers because it is disconnected, making it expensive for some at £20-£30.
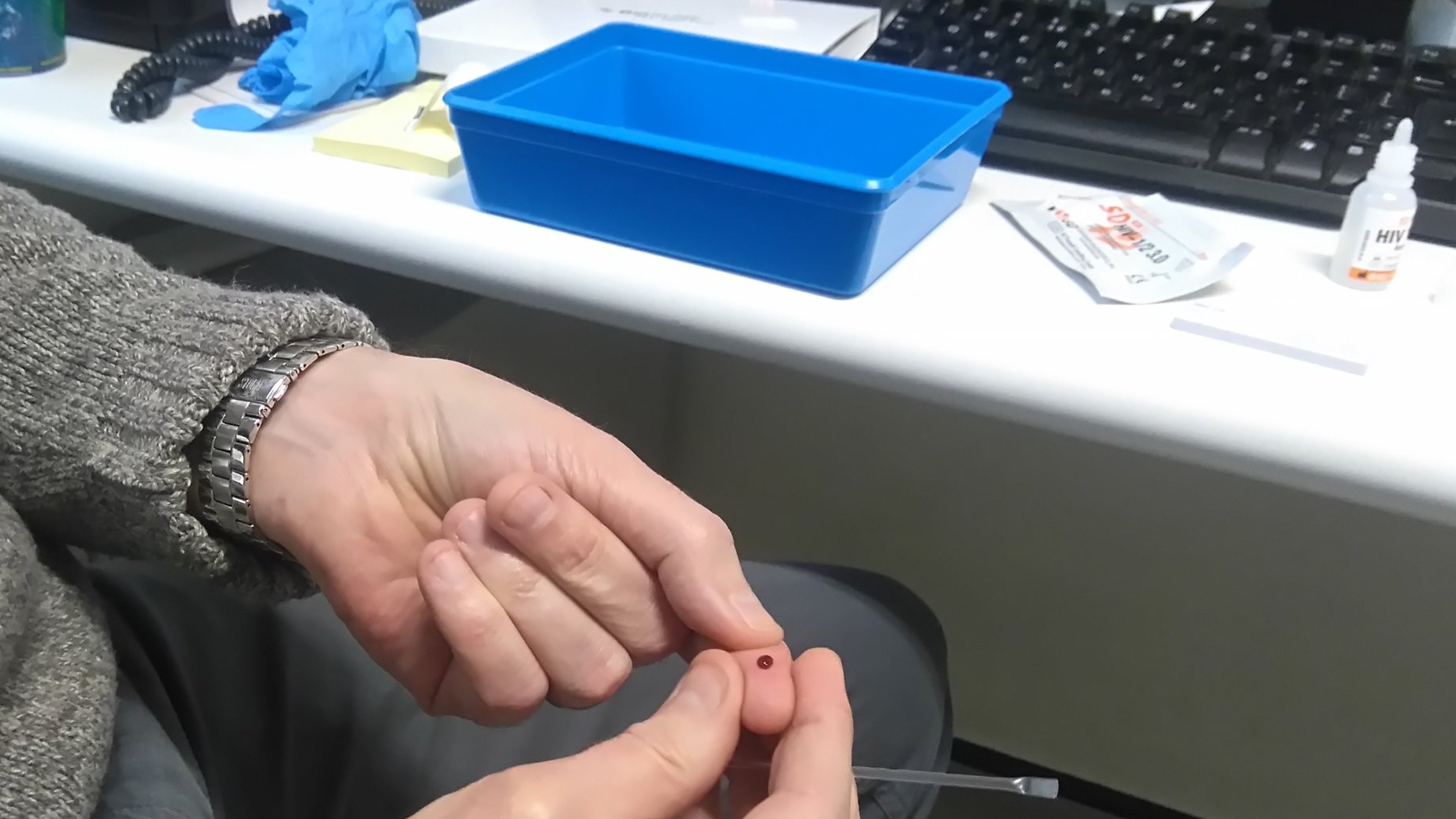
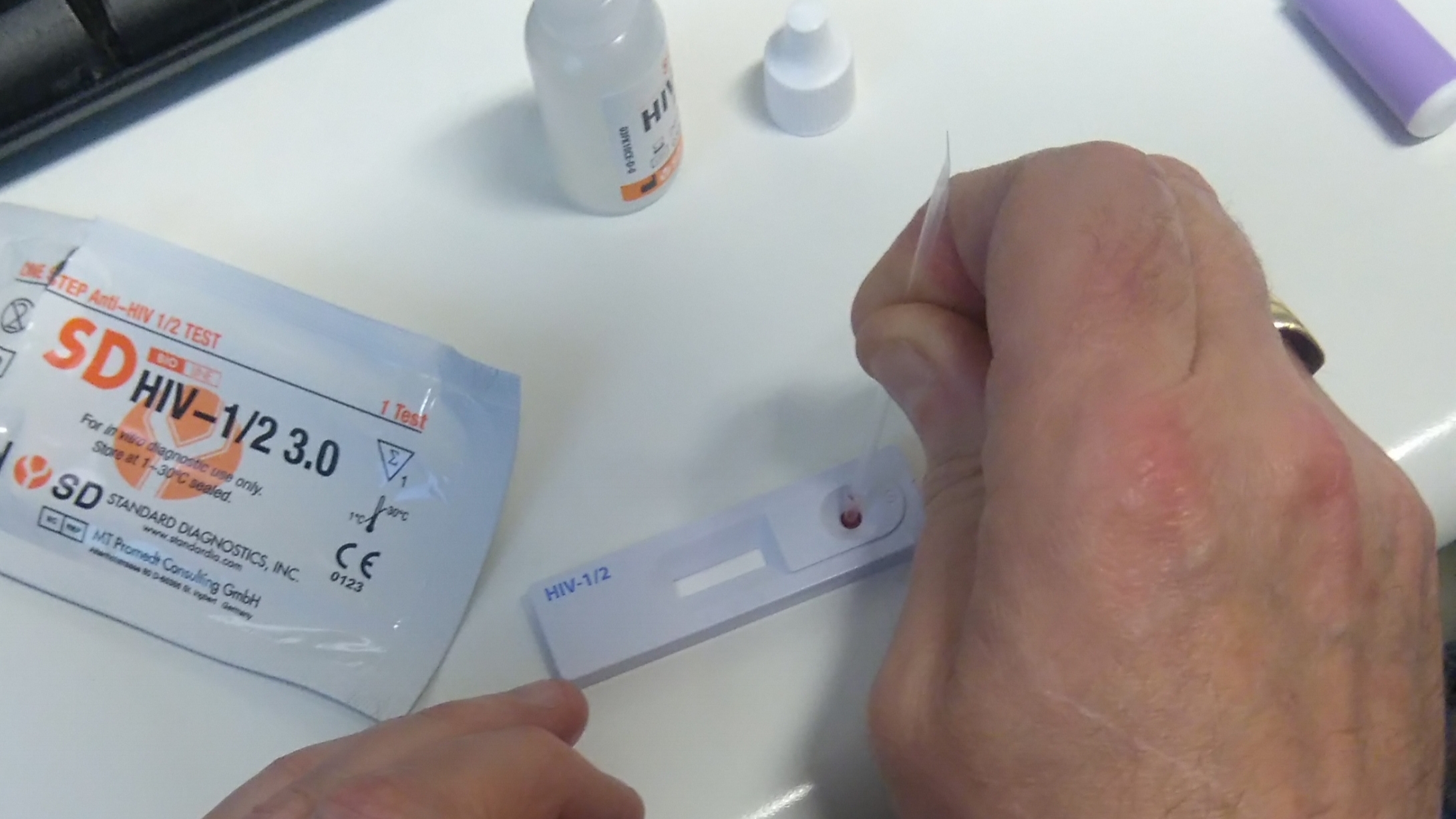
Biosure HIV self-testing kit, a finger prick blood test that gives you a result in 15 minutes.
>>
The solutions
We proposed Just Check which is a sexual health service that makes self-testing accessible and supported, encouraging diagnosis.
Just Check brand image
Below are four interventions of the service:
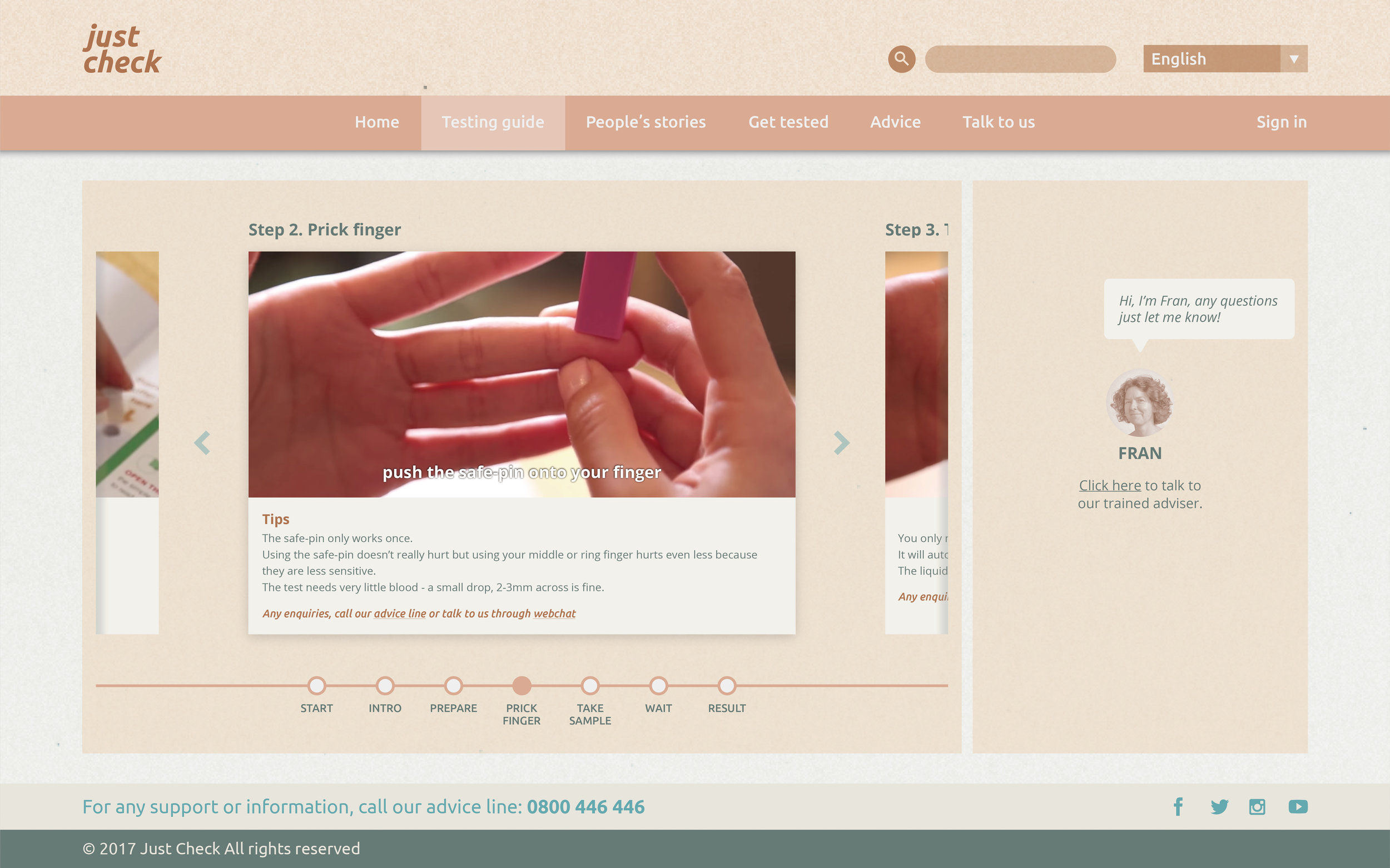
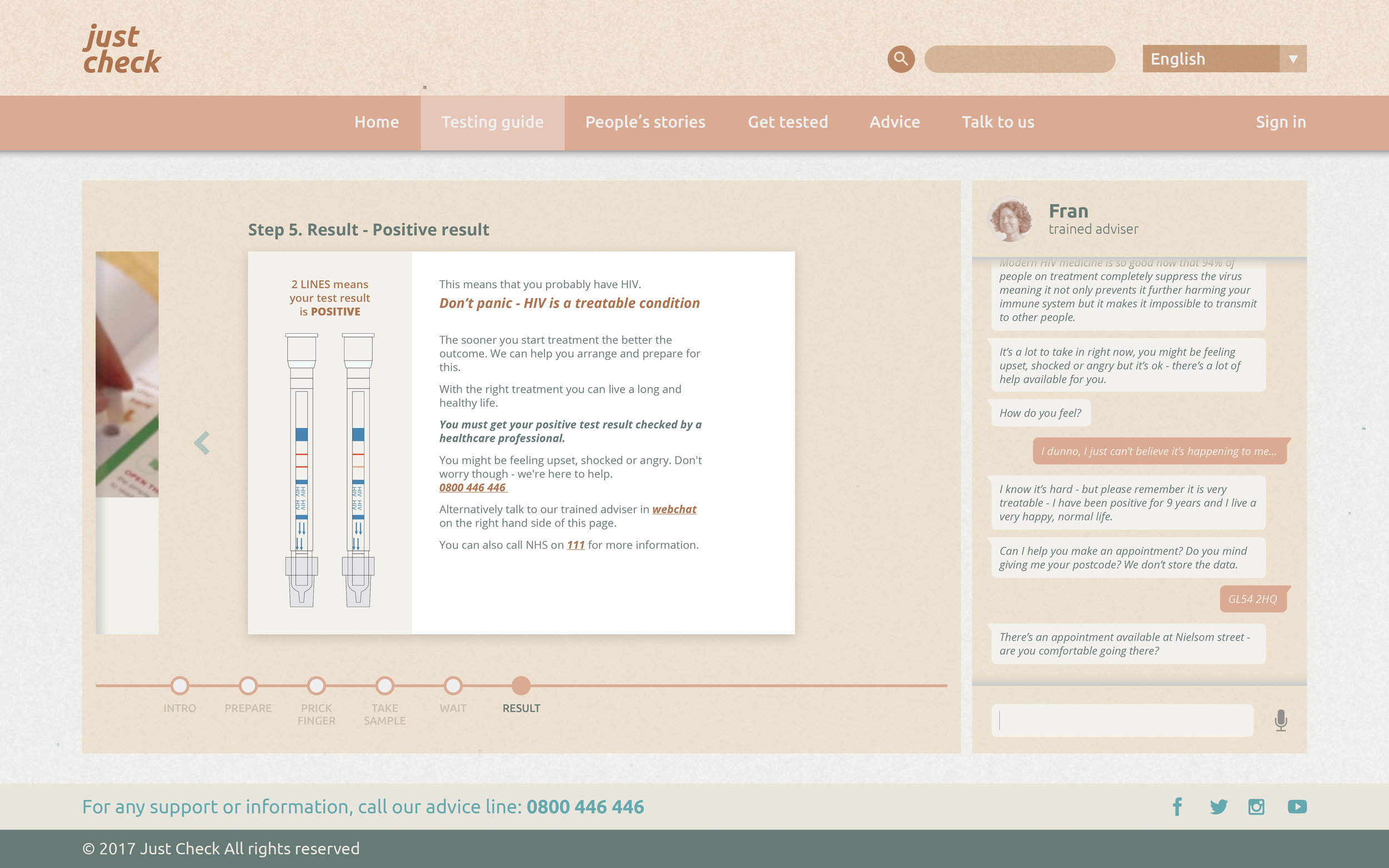
Supported System: Offers people assuring information and support through the testing process, reducing their anxiety.
Promotion Tools: Help charities penetrate further into communities and encourage advocacy, reaching more people at risk.
Onward guidance: Phone and online peer support for those who test positive, preventing panic and connecting people to clinical services.
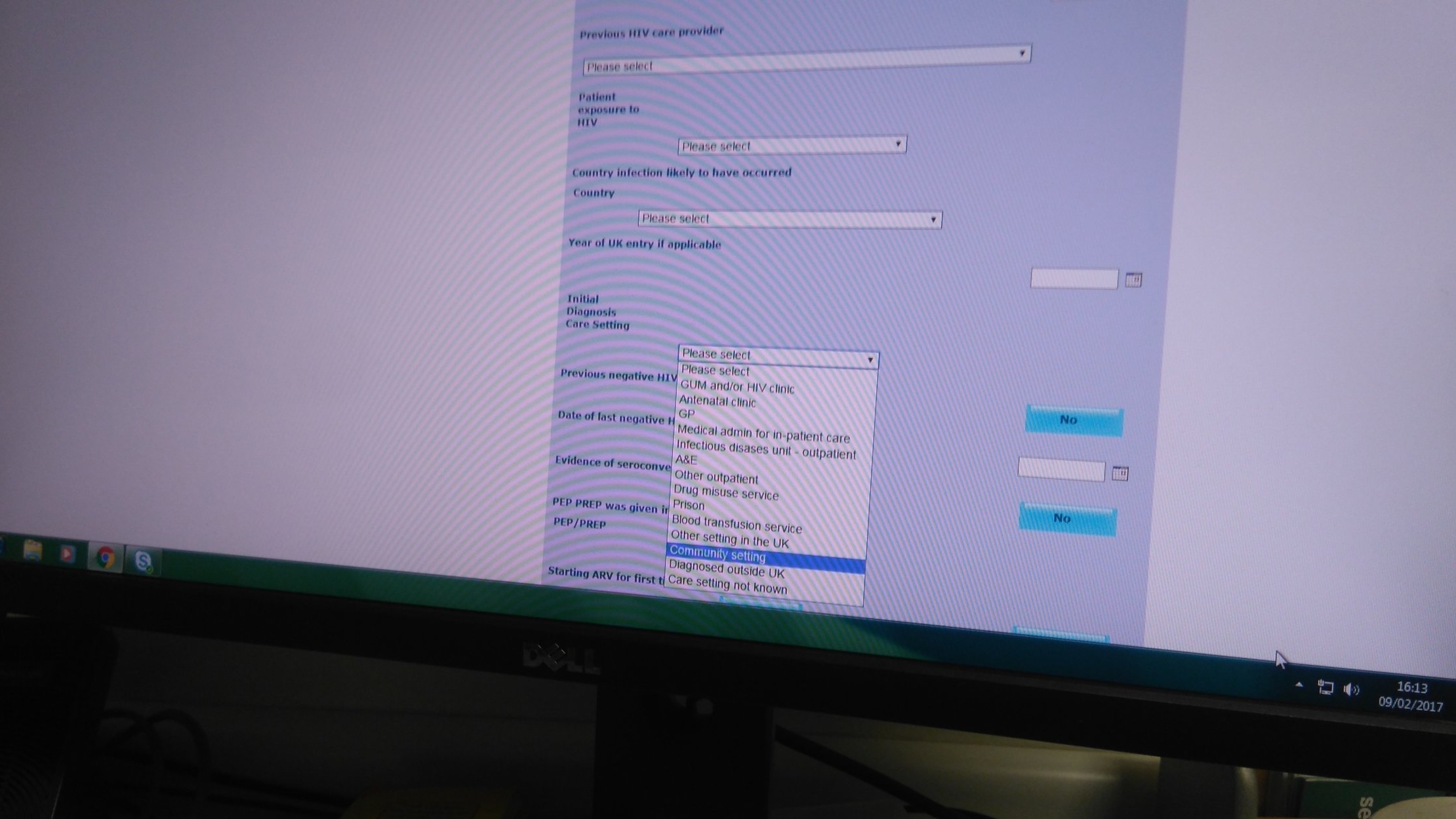
Measurement System: Activation and discount codes to track test use and results, measuring impact and encouraging funding.
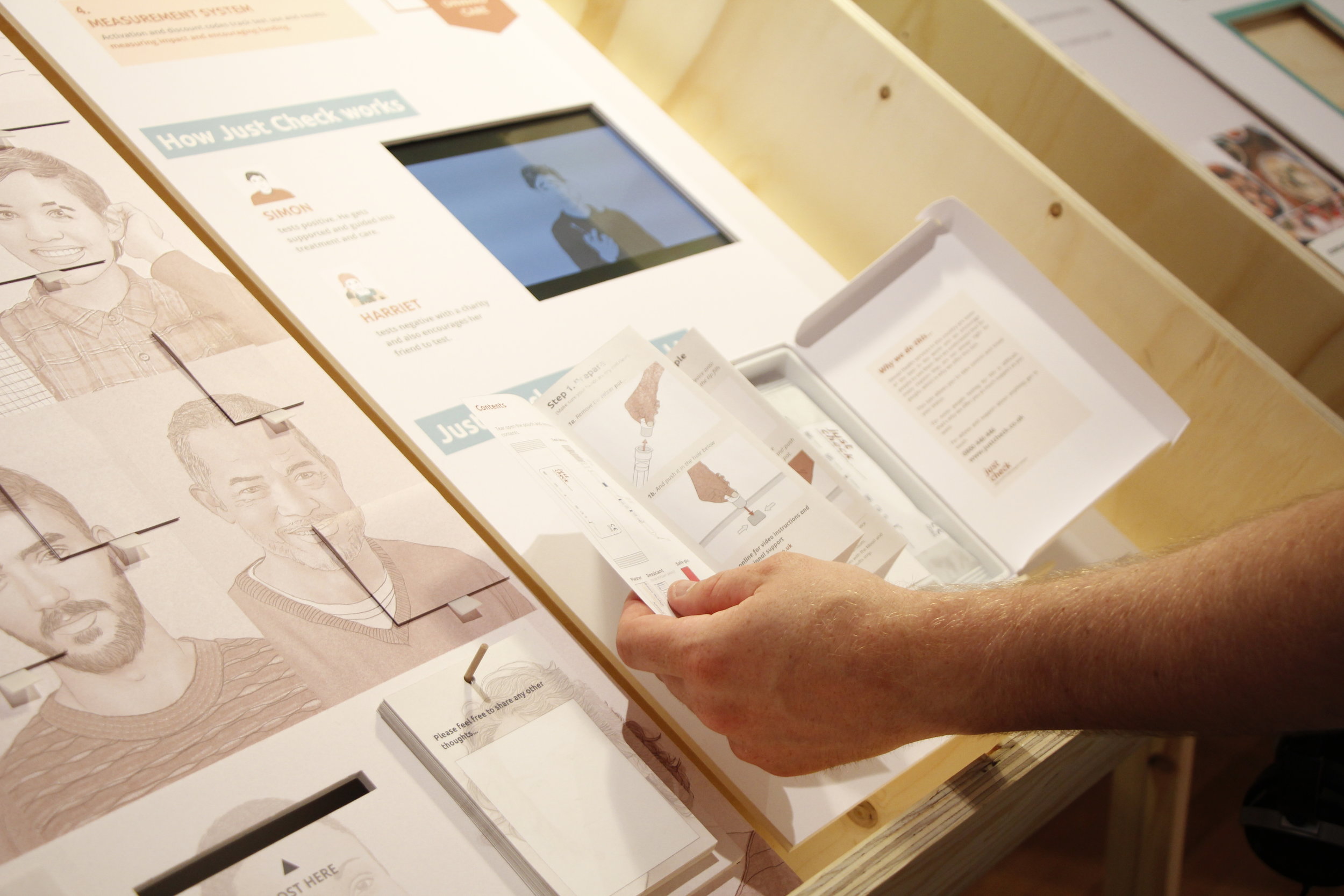
The two stories below demonstrate how Just Check works.
Simon tests positive. He gets supported and guided into treatment and care.
Harriet tests negative with a charity and also encourages her friend to test.
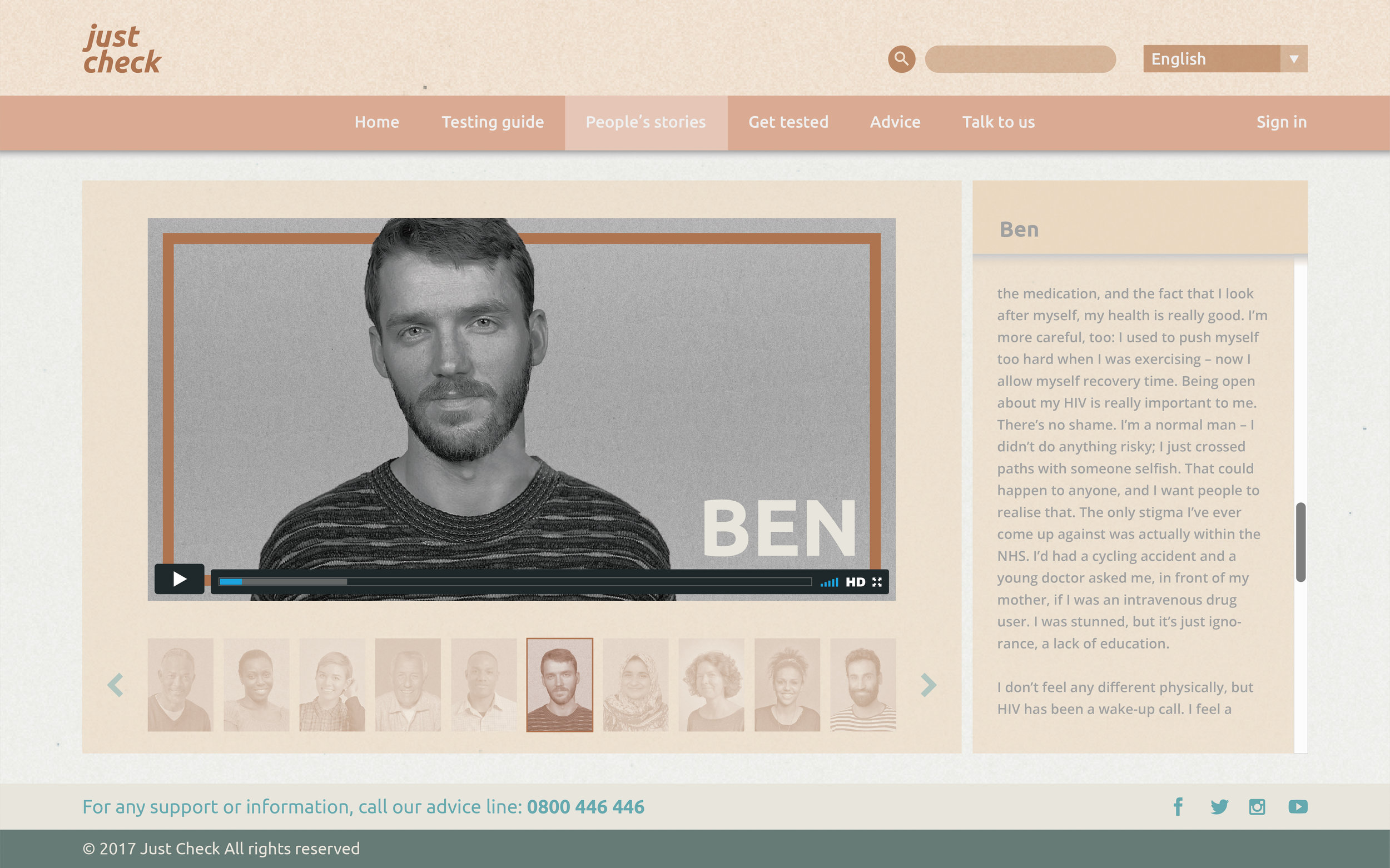
Below are Just Check website and HIV self-testing kit images
>>
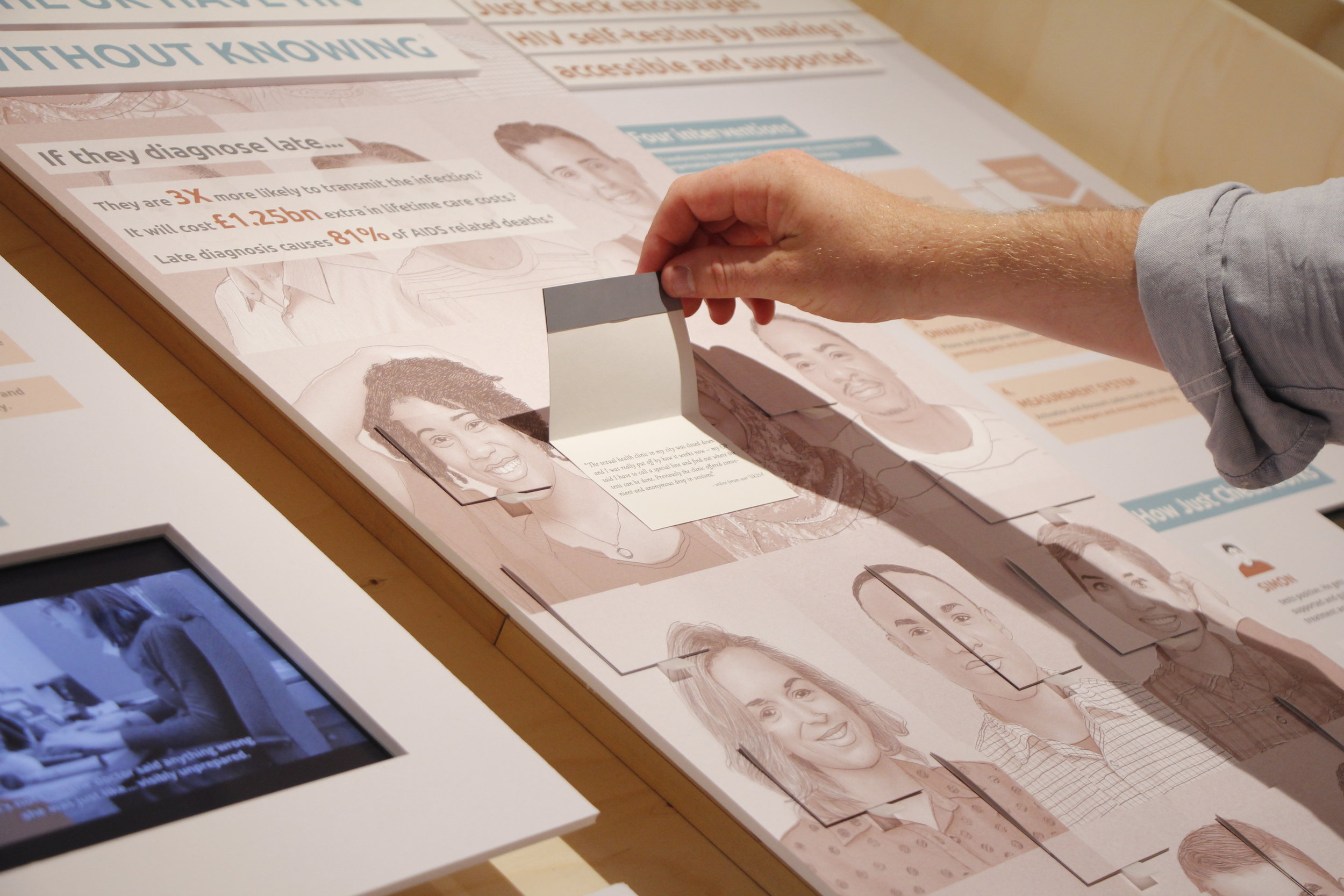
Exhibition of work
The project was exhibited in ShowRCA 2017.
>>
Reference
- United Anger: a history of Act Up. <https://youtu.be/MrAzU79PBVM>
- AIDS: Don't die of ignorance. <https://youtu.be/TMnb536WuC0>
- Public Health England. United Kingdom: National HIV surveillance data tables. (PHE, 2016)
- The National Institute for Health and Care Excellence. HIV testing. (NICE, 2014)
- HIV Prevention England. Undiagnosed HIV infection 2013. (NAM, 2013)
- HIV Prevention England. Undiagnosed HIV infection 2013. (NAM, 2013)
- Public Health England. HIV in UK report. (PHE, 2016)
- Fumiyo Nakagawa, Alec Miners, Colette J. Smith, Ruth Simmons, Rebecca K. Lodwick, Valentina Cambiano, Jens D. Lundgren, Valerie Delpech, Andrew N. Phillips. Projected lifetime healthcare costs associated with HIV infection. (PLOS One 10(4): e01205018, 2015)